
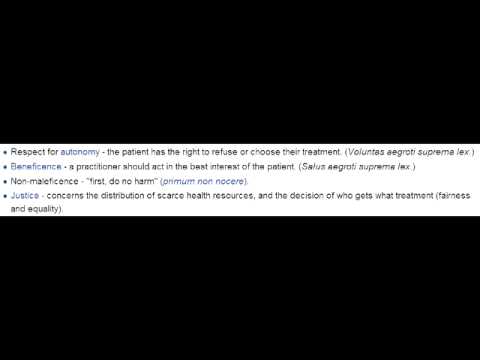
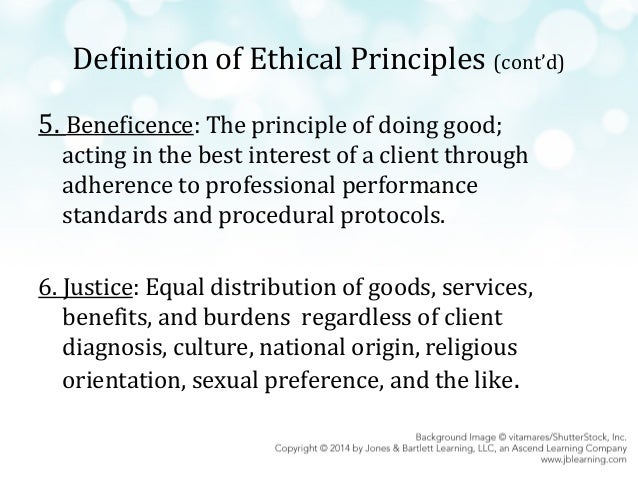
Leaving a patient at home instead of transporting them to hospital when required does not follow the non-maleficence principal. This can include direct physical harm to a patient or failing to consider the possible outcomes of a course of action. The ethical principle of non-maleficence advocates avoiding the cause of undue harm to the patient (Ashcroft 2007). It is therefore in the patient’s best interest to be transported to hospital for further assessment. The duty of care relates to both the beneficence principal of doing good and the non-maleficence principal of doing no harm. According to Butt (2011), a duty of care is the obligation of a person to take care to ensure they are not causing another person to suffer harm. Paramedics have a duty of care to all patients. There is often a medical or psychiatric reason for the patient’s behaviour (Bledsoe 2008). Although it may seem that the patient is not being completely honest, paramedics should exclude all other medical and psychiatric causes before coming to a conclusion. Paramedics must also assume that the patient is telling the truth.
#Beneficence ethical principle manual#
According to the Queensland Ambulance Clinical Practice Manual (2011), definitive diagnosis of a patient cannot always be established in a pre-hospital setting. In this case study, paramedics have to ask themselves if transport will benefit the patient. The ethical principal of beneficence defines the moral obligation of healthcare workers to maximise benefits and minimise harm to patients (Ashcroft 2007, Ruderman 2006). In the instance of “frequent flyers”,especially in this case study, paramedics need to inform the patient that if he goes to hospital he is most likely going to be put out in the waiting room.
This therefore involves consulting patients and getting their permission before anything is done to them (Gillon 1994).
Treatment as long as it is informed decision making, by paramedics giving themĮnough information to make a decision about a treatment, paramedics must then accept the patient’s decision (Sullivan 2000 & Gillon 1994). Whether this is accepting treatment or refusal of
In autonomy, in regards to paramedic practice, paramedics must respect the treatment option the patient chooses. Capacity needs to be decided to see if he is in the right frame of mind or whether he has another issue such as a mental health issue, anxiety, loneliness or if he is just attention seeking. In this patient, seeing whether or not he has the decision making capacity is an important aspect as it will inform the diagnosis (Larkin, Marco & Abbott 2008). To respect a patient’s autonomy specific elements are required these elements include gaining consent, confidentiality, the patient’s capacity, information giving or communication and voluntariness (Sullivan 2000 & Gillon 1994). The concept of autonomy relates to self-government or self-determination and requires two conditions "1) liberty, or independence from a controlling influence and 2) agency, or a capacity for intentional action" (Varelius 2006 Sullivan 2000).


 0 kommentar(er)
0 kommentar(er)
